Diagnosis of COVID-19
Thu, 2020-12-03 23:40Diagnosis of COVID-19
Volume 16, Issue 1, January 2021 (download full article in pdf)
Editorial note
Coronavirus disease 2019 (COVID-19) is undoubtedly the most topical subject not only in the medical field, but also for humanity globally. In this issue of the Topical Update, Dr. Derek Hung and Prof. Kwok Yung Yuen present an overview on the diagnosis of COVID-19, which underpins effective disease control. We welcome any feedback or suggestion. Please direct them to Dr. Janice Lo, Education Committee, The Hong Kong College of Pathologists. Opinions expressed are those of the authors or named individuals, and are not necessarily those of the Hong Kong College of Pathologists.
Dr. Derek HUNG and Prof. Kwok Yung YUEN
Resident, Department of Microbiology, Queen Mary Hospital, Hospital Authority and
Professor, Department of Microbiology, Faculty of Medicine, The University of Hong Kong
Overview
Coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) since December 2019 has infected 54 million population in all six major continents, resulting in over 1.3 million deaths by mid-November 2020. One of the most important aspects in curbing the spread of the virus is rapid yet accurate diagnosis of infection followed by timely isolation and contact tracing. Molecular testing is now the mainstay of diagnosis, supplemented by viral antigen testing. Antibody detection aids in assessment of immunity and disease prevalence in the population. As the disease progresses, there are worldwide efforts in developing a multitude of diagnostic platforms, both in-house and commercial. Studies also endeavour to assess optimal types and timing of specimen collection to enhance diagnostic yield. In this review, we would look at some of the knowledge and practices in making a diagnosis of COVID-19.
Specimen collection
Obtaining the best specimen optimizes the possibility of getting the correct diagnosis based on clinical suspicion. Being a predominantly respiratory pathogen, obtaining respiratory specimens for viral detection remains the primary modality for making a diagnosis of acute infection by SARS-CoV-2. The viral load is highest at or soon after symptom onset, with the viral load in the upper respiratory tract peaking earlier than the lower respiratory tract. The viral load decreases in the respiratory tract at a rate of 1 log10 per week. The World Health Organization (WHO) suggests that testing upper respiratory tract specimens is adequate for early stage infection, especially asymptomatic or mild cases. The Centers for Disease Control and Prevention (CDC) recognizes nasopharyngeal swab, nasopharyngeal wash, nasal wash obtained by health care professionals; nasal mid-turbinate swab, nasal swab obtained by either health care professionals or supervised self-collection on site; and posterior oropharyngeal saliva (POS) by supervised self-collection as valid specimens. Patients with lower respiratory tract symptoms such as productive cough, shortness of breath, or suspicious radiological findings should send sputum to enhance sensitivity. Induced sputum is not recommended due to increased risk of aerosol transmission,. Among different respiratory specimens, broncho-alveolar lavage (BAL) showed the highest positive rate.
For the upper respiratory tract specimen, comparing combined nasal swab/throat swab with nasopharyngeal swab, Vlek et al showed high concordance between these two methods (kappa coefficient 0.95) despite the cycle threshold value (Ct value) obtained from nasopharyngeal swab being lower. Another study suggested nasal swab alone also has good concordance with nasopharyngeal sampling. In contrast, oropharyngeal swab alone has inferior performance. Wang et al showed the sensitivity of oropharyngeal swab was 21.1% and meta-analysis by Bwire et al suggested the positive rate is as low as 7.6% in suspected cases, comparing with 69.6% and 71.3% for nasopharyngeal swab and lower respiratory tract specimen respectively. POS is increasingly studied as an alternative respiratory tract specimen for diagnosis. Theoretically well produced POS can concentrate secretions dripping down from nasopharynx and lower respiratory secretion moved up by ciliary activity of respiratory epithelium. It can be saved by patients themselves with instructions, thus reducing discomfort in specimen collection and minimizing aerosol exposure for health care professionals. The cost of collecting POS could be 2.59-fold lower than nasopharyngeal specimen, which could be significant in resource limited setting. The concordance between POS and nasopharyngeal swab is high, especially in the first 7 days of infection, up to 96.6% positive percent agreement. The sensitivity is comparable with nasopharyngeal swab in properly collected specimen. The sensitivity does not vary much between early morning and at least 2 hours after meal, which provides a convenient option for specimen collection. CDC and Hospital Authority of Hong Kong have adopted POS as an alternative option for upper respiratory specimen collection.
Viral shedding is also found in other specimens with stool being more studied. Meta-analysis showed viral shedding was found in faecal material in 40.5% of patients. The viral shedding in stool is more prevalent in those with gastrointestinal symptoms and may last longer than the shedding in respiratory tract. Viral RNA detected in blood and urine is relatively uncommon, respectively only 1% and 0% in one study with more than 200 patients10. Even without ocular symptoms, the conjunctival secretion may contain a small amount of SARS-CoV-2 RNA in around 8% of patients, warranting appropriate infection control measure in ophthalmological assessment.
Molecular testing
Detection of nucleic acid remains the backbone of diagnosing COVID-19 for treatment and public health purposes. Reverse-transcriptase polymerase chain reaction (RT-PCR) is the most widely used technique. After transcribing the viral RNA into complementary DNA (cDNA) with reverse transcriptase, the cDNA would be amplified and detected by real-time PCR. Potential molecular targets for SARS-CoV-2 include genes encoding structural proteins, e.g. spike (S), envelop (E), helicase (hel), nucleocapsid (N-N1 and N2), transmembrane (M); and non-structural regions, e.g. RNA-dependent RNA polymerase region (RdRp), haemagglutinin-esterase (HE), and open reading frame 1a (ORF1a) and ORF1b. Most scientific institutes and commercial platforms would design primers to target more than one gene, or to target multiple loci of the same gene to enhance diagnostic sensitivity and specificity. Though N gene RNA is shown by nanopore direct RNA sequencing study to be the most abundantly expressed transcript in SARS-CoV-2 infected cells, there is no consensus on which gene confers the best diagnostic performance. Presently, one conserved and one specific target region are recommended to mitigate effect of random mutation or genetic drift while maintaining specificity25. Various regimens for testing are proposed in the literature. Corman et al recommended the Charité protocol, which was to use E gene for screening and RdRp gene for confirmation. CDC used N1 and N2 genes as their diagnostic panel. Chu et al used N gene as screening test and ORF1b as confirmatory assay because the screening N gene assay is 10 times more sensitive than ORF1b. As an alternative confirmatory assay, Chan et al developed a real-time RT-PCR assay locally, targeting RdRp/Hel. This COVID-19-RdRp/Hel assay demonstrated significantly higher sensitivity and specificity for the detection of SARS-CoV-2 RNA than the RdRp-P2 assay in clinical evaluation.
Multiple commercial platforms were developed for molecular SARS-CoV-2 diagnosis for their high throughput, rapid turnaround time and ease of use with automation. Examples are Roche Cobas 6800/8800 system (targets ORF1a and E genes) and Abbott Alinity m SARS-CoV-2 assay (targets RdRp and N genes), where sample preparation, genetic material extraction, target amplification and result reporting are automated inside the system. Molecular point-of-care testing (POCT) refers to diagnostic platform that is portable (often desktop-size), requires minimal sample preparation steps and can provide reliable molecular results within 2 hours. POCT like Cepheid GeneXpert (Xpert Xpress SARS-CoV-2 assay, targets E and N2 genes) enables rapid testing near the site of collection in areas with little laboratory support. Fewer steps in manipulation reduce risk of cross contamination and laboratory error in processing. Many evaluation studies have been published to compare the performance of these commercial platforms against in-house diagnostic tests and for head-to-head comparison between platforms. For example, Cobas system is shown to have high diagnostic agreement with in-house molecular assays,, as well as with other commercial platforms such as Hologic Panther Fusion system and Cepheid GeneXpert. Cepheid GeneXpert reaches an agreement of 100 % compared to three in-house RT-PCRs in a multicentre evaluation in the Netherlands. Among commercial platforms there might be minor discordance between assays at very high Ct values and the viral load of clinical samples used in evaluative studies should be noted in particular.
Another molecular technique is reverse-transcriptase loop-mediated isothermal amplification (RT-LAMP) test. Using multiple primers for the genetic target, RT-LAMP amplified nucleic acid by strand displacement in an isothermal condition of around 60- 65oC. It allows synthesis of large amount of genetic material up to 106 to 109 copies of target DNA within 30-60 minutes2. Without the need of thermal cycler as in RT-PCR, RT-LAMP facilitates development of rapid molecular POCT and has an expanding market in commercial diagnostic platform. On the down side, since multiple primers over a relatively small genetic region are needed for amplification, there are constraints in properly designing the primers. Abbott ID NOW is a commercial POCT platform using RT-LAMP, allowing real time detection of SARS-CoV-2 within 15 minutes targeting RdRp gene. Evaluation of ID NOW against other RT-PCR based platforms appears suboptimal in terms of diagnostic sensitivity. Compared to Cobas, ID NOW achieved only 73.9% positive agreement while GeneXpert achieved 98.9% positive agreement. In samples with Ct values greater than 30, positive agreement was 34.3% for ID Now and 97.1% for GeneXpert. A lower sensitivity of ID NOW over GeneXpert was also reported in another evaluation by Basu et al. In contrary, good diagnostic utility has been demonstrated in many other centres including Hong Kong that have designed their own RT-LAMP for COVID-19. Chow et al reported sensitivity of 95% at 60 minutes using RT-LAMP targeting a region across ORF3a/E gene as compared to RT-PCR. Lu et al achieved concordance rate of 93% against RT-PCR using in-house E gene RT-LAMP assay.
In order to improve the diagnostic sensitivity of molecular assays, clustered regularly interspaced short palindromic repeat (CRISPR)-based technology has been employed by coupling with Cas enzyme. The enzyme would be directed to the target DNA/RNA by a guide RNA complementary to the target sequence. Once bound, the collateral nuclease activity of the Cas enzyme would cleave surrounding reporter fluorophore and lead to signal amplification. DETECTR technology uses Cas12a enzyme to bind target DNA; while SHERLOCK technology uses Cas13a enzymes to bind target RNA. This technology can be incorporated in molecular techniques especially RT-LAMP to enhance the sensitivity and to lower the detection limit.
Next generation sequencing (NGS) enables sequencing of the entire genome in a relatively short period of time. Sharing of genetic data facilitates tracking of disease spread, understanding of disease transmission route, monitoring viral genome evolution and detecting emergence of mutation that may escape detection or enhance virulence. The cost and infrastructure required of NGS and the need of bioinformatics expertise limit its use to larger hospital and research centres.
Antigen detection
Like other respiratory viruses such as influenza and respiratory syncytial virus (RSV), direct antigen detection from respiratory specimen especially nasopharyngeal sample is another way of making a diagnosis of COVID-19. N protein was found previously to be the predominant structural protein released in large amount in nasopharyngeal aspirate during infection of SARS-CoV, and the same phenomenon is also shown in SARS-CoV-2 where the abundantly expressed N protein is widely used as an antigen detection target in COVID-19. Detection is achieved by capturing viral antigen in clinical specimens by monoclonal antibodies or monospecific polyclonal antibody fixed on a membrane, usually indicated by colour change of the strip in colorimetric lateral flow immunoassay. The assay can be delivered as POCT in an office setting since no complex laboratory support is required and the result can be available within a short period of time, usually <30 minutes. The major setback is the suboptimal sensitivity as compared to molecular diagnosis especially in samples with high Ct values. Evaluation by Lambert-Niclot et al using COVID-19 Ag Respi-Strip CORIS, a nitrocellulose membrane technology with colloidal gold nanoparticles sensitized with monoclonal antibodies directed against SARS-CoV-2 nucleoprotein (NP) antigens, showed sensitivity of only 50% when compared against multiple RT-PCR platforms. For samples with Ct value <25, the sensitivity is higher at 82.2%. In a local evaluation using Biocredit COVID-19 Ag test, the antigen test is 105 fold less sensitive than RT-PCR and it yielded a positive result in 45.7% RT-PCR positive combined nasopharyngeal swab/throat swab specimens only. There are attempts to improve sensitivity of rapid antigen assay. Porte et al evaluated an immune-chromatographic antigen assay using fluorescence signal showing sensitivity of 93% but the Ct value of the sample included in this study is relatively low with mean of 20. Other approaches by concentrating the antigen in specimens before testing with monoclonal antibodies targeting multiple different epitopes of the antigen were also reported. Based on a meta-analysis by Dinnes et al, the average sensitivity is around 56.2% for antigen assay with a high average specificity of 99.5%. Further refinement in antigen detection employs the detection of the change in bioelectric property by antigen binding to the antibody coated membrane. In Seo et al, anti-S antibody binds to SARS-CoV-2 particles to fabricate graphene-based field-effect-transistors (FET) biosensors and can respond down to 16 pfu/mL of virus. One challenge to this advance is the high background noise which can reduce sensitivity of detection. Overall, rapid antigen detection serves only an adjunctive role to molecular assay in making a diagnosis especially in outbreak situation where prevalence is high and molecular assay is not available. WHO has issued interim guidance of use of rapid antigen immunoassays.
Antibody detection
While antibody testing may not be useful in acute setting for COVID-19, it helps establish retrospective diagnosis, predict immunity and understand seroprevalence in a defined community. Commonly employed techniques are lateral flow immunoassay, chemiluminescent immunoassay, immunofluorescent assay, and enzyme-linked immunosorbent assay (ELISA). Median seroconversion times following symptom onset are 11 days for total antibodies, 12 days and 14 days for IgM and IgG respectively. Detection rate for IgM ranges from 11-71% in the first 7 days of infection, 36-87% between 8-14 days, and 56-97% after 14 days. For IgG, it ranges from 4-57% in first 7 days, 54-88% between 8-14 days, and 91-100% after 14 days. For SARS-CoV-2, there does not seem to have significant time difference between IgM and IgG response. IgM peaked at around 3 weeks after symptom onset and fell to baseline level at around day 36. The duration of IgG seropositivity remains unknown and longer longitudinal studies are required. Study from Iceland involving over 1200 confirmed patients showed no evidence of antiviral antibody decline by 4 months after diagnosis; and most other studies showed persistently detectable antibodies by 2-3 months after infection60. On the other hand, there are some evidences that the IgG level may decline faster in mild and asymptomatic61 COVID-19 cases.
S protein is an important antigen for neutralizing antibody production. The S1 domain is responsible for receptor binding while the S2 domain is responsible for fusion. The receptor binding domain (RBD) is located at S1. NP, which is a structural component of the helical nucleocapsid, also appears to be an important antigen for the development of serological assays to detect COVID-19. Earlier in the pandemic, using sera collected more than 14 days after symptom onset from 16 patients, To et al showed rates of seropositivity were 94% for anti-NP IgG, 88% for anti-NP IgM, 100% for anti-RBD IgG, and 94% for anti-RBD IgM. Another study compares sensitivity and specificity in testing anti-S and anti-NP IgG for evidence of immunity across multiple platforms, which shows they are comparable by day 37 after infection though seroconversion of anti-NP IgG may precede anti-S IgG by around 2 days (day 9-10 v day 11-12). Caruana et al observed that the decline of anti-NP antibody may be faster than anti-S and thus could be less sensitive longer after infection. Also titre of anti-S antibody may better reflect protection against reinfection67. Multiple commercial platforms were developed for high-throughput antibody testing in clinical laboratory. Automatic platforms such as Abbott SARS-CoV-2 IgG, which is a chemiluminescent micro-particle immunoassay, are also used in public hospital of Hong Kong for a shorter turnaround time.
Neutralization antibody test is important in assessing in vitro the functional capacity of the humoral response of COVID-19 patients to prevent reinfection by the virus. Traditional neutralization assay such as microneutralization and plaque reduction assay require manipulation of live virus and necessitate biosafety level 3 laboratories. As a result, pseudovirus neutralization assay has been developed. Vesicular stomatitis virus (VSV) expressing S protein of SARS-CoV-2, containing the RBD, is used so that the assay can be performed in biosafety level 2 facilities. SARS-CoV-2 neutralizing antibody starts to rise at around 7-10 days after symptom onset and the median peak time is 33 days after symptom onset. The neutralization titres then decline in 93% of the patients and by a median level of 35% over 3 months. Patients with more severe disease requiring ICU admission have accelerated and augmented neutralizing antibody response compared with non-ICU cases. In non-severe cases who have low peak neutralizing antibody titre, neutralizing antibody level might return to baseline within 2 months. Another clinical use of neutralization assay would be to confirm potentially false positive SARS-CoV-2 serology result. Three children with Kawasaki disease without symptoms or epidemiological linkage to COVID-19 were tested positive to anti-RBD and anti-NP antibodies by a microparticle-based immunoassay but were confirmed negative by microneutralization test.
Studies have shown there are serological cross-reactivity between SARS-CoV-2 and SARS-CoV. Testing sera taken from COVID-19 patients by ELISA, cross-reactivity is seen against S protein and RBD of SARS-CoV, though the intensity of cross-reaction against RBD is weaker than S protein. For the full length S protein, the amino acid sequence homology between SARS-CoV-2 and SARS-CoV is around 75%. The homology between them for RBD which is located in S1 domain is around 74%. For the receptor binding motif (RBM) of the RBD where the virus directly binds to angiotensin-converting enzyme 2 (ACE2), the homology is only 50%. The degree of amino acid homology explains the difference in the level of cross-reaction between them on ELISA. Chia et al showed even more significant cross-reactivity between SARS-CoV-2 and SARS-CoV antibody against NP by Luminex assay than antibody against S1 or RBD as the homology between the NP of these 2 viruses is around 90%. Despite some cross-reaction between antibodies against RBD on ELISA, there does not seem to have significant cross neutralization effect73. Only 1 out of 15 COVID-19 sera showed cross neutralization with SARS-CoV at very low titre. Overall the effect of cross-protection in vaccination and whether antibody-dependent enhancement effect would be seen between these 2 closely related viruses remains unknown.
Cross-reactivity against other human coronaviruses in SARS-CoV-2 infection has been investigated in a few trials. In a study by Wölfel et al, using immunofluorescence assay against recombinant S protein, cross-reactivity of SARS-CoV-2 sera is found against human coronaviruses OC43, NL63, HKU1 and 229E on comparing the titres between admission and convalescence samples, especially HKU1 and OC43 which are both betacoronavirus. In Shrock et al, deep serological profiling of sera from SARS-CoV-2 patients and pre-COVID sera are performed. Antibodies against S and NP are the most specific assay to differentiate SARS-CoV-2 and pre-COVID sera. Those with dramatic increase in anti-S antibody after COVID-19 infection also have increase in the intensity of cross-reactivity against other human coronaviruses, especially over more homologous regions of the S protein e.g. at residue 811-830 and 1144-1163. It could be novel antibodies of SARS-CoV-2 that cross-react or boost the anamnestic response against SARS-CoV-2 infection due to existing memory towards other human coronaviruses from past exposure. Moreover, pre-COVID sera also show some cross-reaction towards the homologous region of SARS-CoV-2 S protein and ORF1 in the same study.
Viral culture
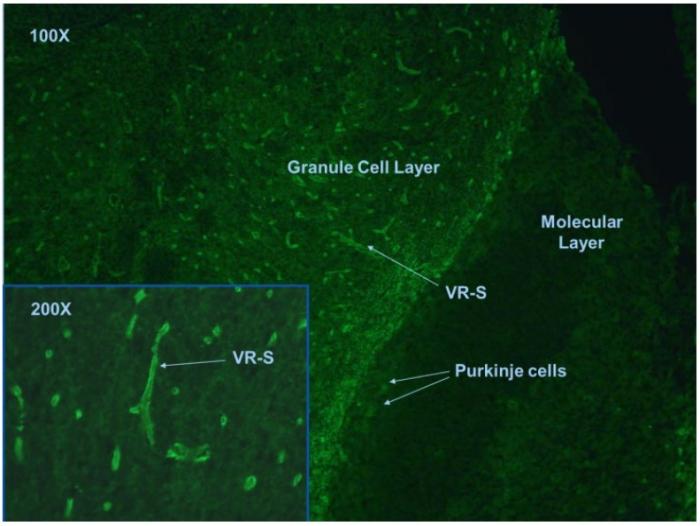
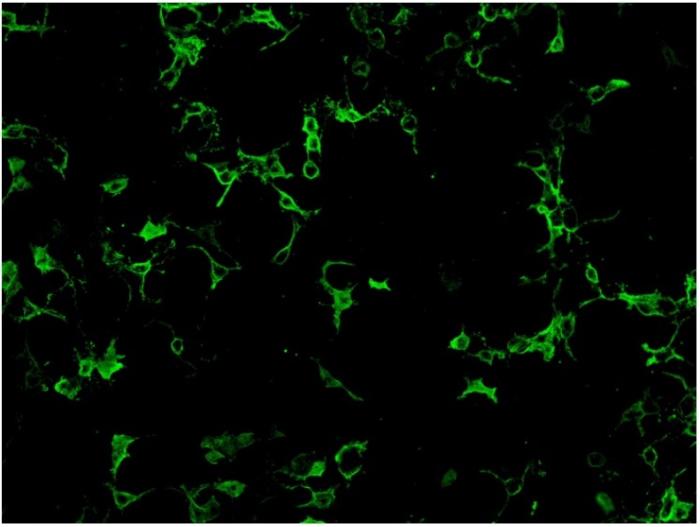
Demonstration of live SARS-CoV-2 in cell culture requires biosafety level 3 facilities and are not routinely performed in most of the clinical laboratories. However, live virus isolation is still important for some diagnostic and research purposes so as to determine whether the amount of virus present is infectious to others, to evaluate therapeutic efficacy of potential antiviral compound, to develop viral neutralization assay for testing convalescent sera, to provide positive control for molecular assay development, and to develop vaccine strains. The host cell receptor for SARS-CoV-2 is ACE2. Non-human cell lines such as Vero E6 and Vero CCL-61 which have abundant ACE2 expression are commonly used for isolation. Cytopathic effect is seen by 3 days after inoculation. SARS-CoV-2 also grows in human continuous cell lines such as Calu3 (pulmonary cell line), Caco2 (intestinal cell line), Huh7 (hepatic cell line), and 293T (renal cell line). It grows modestly on U251 (neuronal cell line) which is not seen in SARS-CoV81. Confirmation of SARS-CoV-2 replication in the cell line can be done by molecular testing or immunostaining techniques. Cell lines can be engineered to express a transmembrane serine protease TMPRSS2 for priming of S protein and to facilitate the entry of SARS-CoV-2 into host cell. Organoid systems such as bat and human intestinal organoids are susceptible to SARS-CoV-2 and are developed to better study tissue tropism, the dynamics of infection and testing of therapeutic targets.
Radiological diagnosis and artificial intelligence
There are no pathognomonic radiological features on chest imaging for COVID-19 and the disease should not be ruled in or ruled out based on imaging alone. However, presence of suggestive imaging features can prompt further investigations in suspicious cases, such as lower respiratory tract viral testing for confirmation. Reports in literature have suggested that in some patients, radiological findings may precede the detection of SARS-CoV-2 in clinical specimen,. Chest X-ray (CXR) is a less sensitive modality than computed tomography of the thorax (CT thorax) with a reported CXR sensitivity of 69%85. As in other viral pneumonia, COVID-19 typically presents with multifocal air-space disease, especially with a bilateral lower lung distribution. More specific to COVID-19, it tends to have peripheral lung involvement, seen in 58% of CXR in one study. CT thorax has a higher sensitivity than CXR, quoted at around 60-98%. CT thorax often demonstrates the typical findings of peripheral bilateral ground glass opacities (GGO) with or without consolidation or ‘crazy-paving pattern’. Sometimes the GGO would arrange in a rounded pattern. Isolated lobar or segmental consolidation without GGO, centrilobular shadows, cavitory changes, lymphadenopathy and pleural effusions are rare86. As the disease advances, the opacities might coalesce, affecting central and bilateral upper lobes and may manifest as ‘white lung’ with diffuse infiltrate. The abnormalities usually peak by 2 weeks after symptom onset, replaced by scar tissue with recovery. In the COVID-19 pandemic, artificial intelligence (AI) programme is increasingly studied for screening abnormal radiological result which would be particularly useful for mass screening strategy in outbreak situation. The performance of AI is dependent on the radiological imaging algorithm being fed into the system for deep learning process. So far the result of this research has been promising with reported area under receiver operating characteristic curves greater than 0.9,. However, there are still lots of technical and ethical issue to resolve which include dataset bias, data privacy, and the distribution of ultimate accountability of result.
Detection of host inflammatory reaction
In COVID-19, there are studies to diagnose and predict severe diseases by the host inflammatory response. Apart from direct viral damage, uncontrolled cytokine storm triggered by the virus leads to tissue damage and multiorgan failure. Mean interleukin-6 (IL-6) concentration in serum was found to be 2.9 fold higher in patients with complicated COVID-19 disease than non-complicated disease. It became one of the markers clinicians could use to predict progression into severe disease. Roche Elecsys IL-6 immunoassay received FDA Emergency Use Authorization to help identify patients at high risk of requiring intubation with mechanical ventilation. Molecules targeting IL-6 such as tocilizumab are also studied as therapeutic to prevent disease progress by blocking the inflammatory pathway. It does not show efficacy in preventing intubation or death in moderately ill hospitalized patients in the BACC Bay trial. Elevated CRP is associated with worse outcome, as well as elevated IL-10 which may be related to compensatory anti-inflammatory response and secondary infections. Haematologically, severe disease is associated with higher absolute neutrophil count, D-dimer and LDH but lower absolute lymphocyte101 and platelet count.
Conclusion
Global COVID-19 pandemic stimulates global effort in development of rapid yet accurate diagnostic techniques. Diagnosis is often limited by the low level of viral particles in the specimen and the subtle clinical features in early infection. Though traditional methods like RT-PCR are still the mainstay, we see expanding endeavours to strive for higher speed and lower limit of detection at an earlier time. Molecular techniques such as RT-LAMP, CRISPR/Cas, biosensor technology in antigen detection, AI operating system for image interpretation are pushing the diagnostic ability to the limit. Despite these scientific advances, there are still a lot of gaps to fill especially in understanding the nature and duration of humoral immunity response and its protection against re-infection. All these require continuous global cooperation and information exchange to make them possible.